Terminology
Introduction
Consensus on terms, definitions and classification is important for any surveillance system and enables the sharing of information internationally. It also facilitates international comparison of surveillance system outcomes in terms of trends, risk groups and patterns of aftercare. This in turn will facilitate international collaboration with regard to building an evidence base for interventions, prevention programs and best practices for people at risk of, and engaging in, suicide attempts and self-harm.
- Shared terminology, definition and classification of suicide and suicide related phenomena is an on-going challenge (8, 9, 10).
- Variation in nomenclature, recording procedures and classification of suicide is associated with the lack of reliable and accurate suicide statistics (e.g. under-reporting of suicide in countries where suicide is criminalized) (9, 11).
A Brief History of Terms
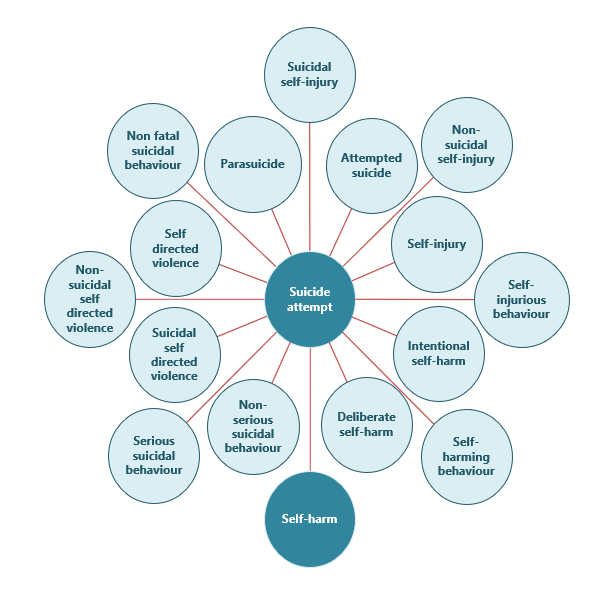
Research into the epidemiology and etiology of suicidal behavior is hampered by the lack of agreement on terminology and definitions. Over the years a wide range of terms have been used to indicate types of intentional self-harming behavior with varying degrees of suicidal intent and varying underlying motives – such as “self-injury”, “parasuicide”, “attempted suicide”, “deliberate self-harm” and “self-harm” (see Figure 1.1 (12)). Reaching agreement on terminology and definition is further complicated by the varying levels of suicidal intent and heterogeneity of motives reported by people engaging in self-harming behavior.
The complexity in deciding on the most suitable term is related to intent to self-harm, which to some extent has to be present in order to classify an act as non-accidental. Consequently, a very fine line has to be followed, where suicidal intent is recognized as fundamental to naming an act as non-accidental yet the term cannot carry the sense of suicidal intent only because this also involves a wide range of other motives, such as relief from unbearable thoughts, self-punishment and seeking attention (13, 14, 15).
Terminology such as “non-suicidal self-injury” (NSSI), recently introduced as a diagnostic category in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), may be an appropriate concept within clinical practice but may not represent appropriate terminology for surveillance (16). For example, the diagnostic criteria for NSSI state that the person has engaged in self-injury for at least five days. When collecting data for the surveillance system, this information may not be known or be obtainable.
Furthermore, evidence shows suicidal intent to be a fluid rather than a dichotomous “either/or” concept. Any descriptor term that takes a side in the either/or argument by excluding or including ideas of intent becomes problematic because it has the potential to exclude a section of the self-harm population (17, 18).
